When I first designed my project, my goal was to improve outcomes for patients with diabetes and hypertension by leading targeted outreach. The plan centered on hosting educational sessions with certified diabetes educators and local chefs who could demonstrate how to adapt cultural cuisines into healthier meals. To expand the impact, I also intended to create and distribute educational pamphlets, ensuring even patients who could not attend sessions had access to practical lifestyle guidance.
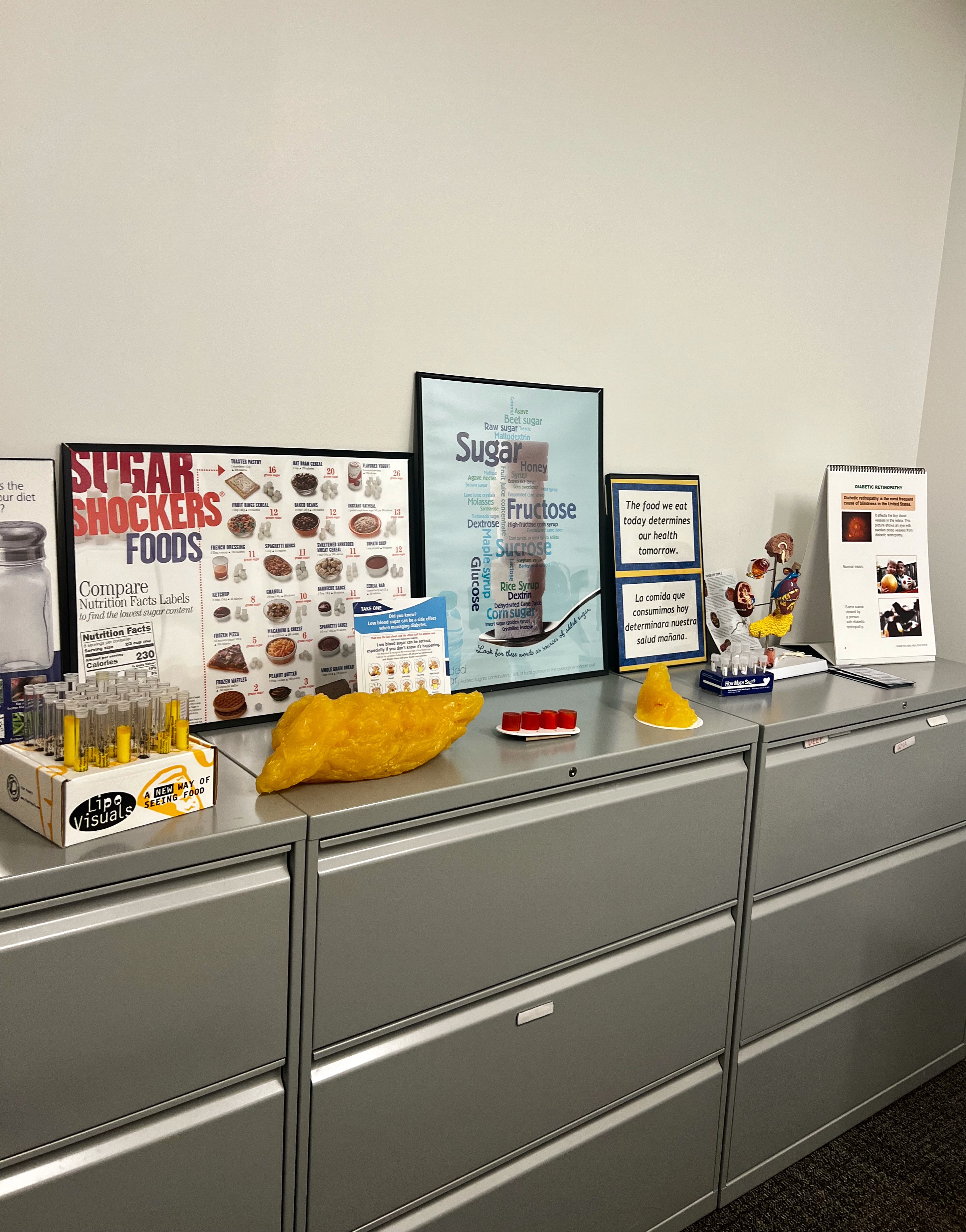
Once I began working at Samuel Rodgers, however, the project quickly evolved to meet the health center’s more immediate needs. In my first week, I shadowed the Population Health team, who work closely with patients through the Medicare Health Home initiative. Sitting in on clinical appointments and follow-up goal-setting sessions revealed a key principle: meet patients where they are. I saw how staff balanced evidence-based guidance with the realities of patients’ stressors, food access, and cultural values. Additionally, I saw how the Population Health team dedicated significant time to walking patients with diabetes or hyperlipidemia through their diets and identifying healthier alternatives to their favorite foods that still aligned with their health goals. From this, I learned effective strategies for patient engagement and was able to apply them myself in conversations with patients.
This perspective came into sharp focus when I learned about the Prescriptive Pantry program, which once provided fresh foods tailored for diabetic patients but had recently paused. I helped the team organize and relabel the pantry’s remaining inventory and prepare for a fall 2025 relaunch with the support of Harvesters, a regional food bank. Patient feedback was overwhelmingly positive, with many asking when the program would be fully up and running again. For many, it helped provide more consistent and nutritious meals, especially since healthier foods tend to be less accessible. Witnessing how access to food directly shaped patients’ health brought the mission of Samuel Rodgers, removing barriers to care, into daily life.
Midway through the summer, I also worked alongside the Outreach team. At the Mexican Consulate, we offered free blood pressure checks and lipid panels to community members, many of whom traveled hours from other states. Explaining results and sharing information about Samuel Rodgers’ services showed me how outreach bridges trust and accessibility, especially for immigrants navigating new systems. I later supported our annual Back-to-School event, which not only provided school and hygiene supplies but also connected families to health, vision, and dental services. This illustrated how holistic care strengthens community wellbeing.
In the final weeks, my focus shifted again to colon cancer screening, where the center saw an urgent gap. I identified patients overdue for colonoscopies and spoke with them (in both English and Spanish) about screening options, including free Cologuard kits. Language skills made a significant difference here. Most of these conversations happened in Spanish, which pushed me to adjust to different accents and dialects. I saw firsthand how patients became more comfortable once I spoke to them in Spanish if it was their preferred language. They opened up about their experiences, such as already having a screening kit but feeling unsure about how to use it or where to send the sample. I was able to address these concerns and help clarify the process for them. These conversations underscored how culturally and linguistically competent care empowers patients to take preventive action. Moreover, it reinforced just how powerful it is when patients feel both informed and heard.
Across these eight weeks, my project expanded far beyond educational sessions and pamphlets into a multidimensional experience of population health. By adapting to the center’s priorities such as food security, outreach, and cancer prevention, I was able to contribute in ways that directly supported Samuel Rodgers’ mission to provide accessible, community-centered care. More importantly, I saw firsthand how small acts, whether organizing food boxes, explaining lab results, or handing out water on a hot day, can ripple into meaningful health improvements.